
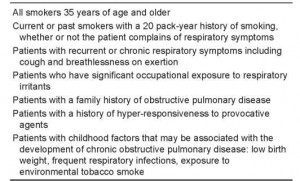
Recently, Chan et al looked at spirometry use in Ontario and reported a rapid increase in its use due to the diffusion of inexpensive spirometers in physicians’ offices and an increased awareness of guidelines promoting objective testing. However, there was a wide regional variation in spirometry use. A corresponding editorial by Anthonisen suggested that these overall rates of use were a blunt instrument for health care utilization analysis. What we really need to know is whether the right patients are being screened, diagnosed or followed with this tool. A reasonable approach for surveillance spirometry based on the results of the Lung Health Study is to screen all smokers over 35 years of age. If this model seems too onedimensional, COPD screening can also be conceived in the context of a matrix that sifts a few straightforward risk factors with the complex pathophysiology of the disease. Smoking is the major risk factor for COPD, but only a small percentage of smokers are at risk. Age is a factor, but significant airway limitation may be present in younger, asymptomatic patients. Methacholine reactivity is a factor, but it is linked to smoking and airflow limitation and does not necessarily indicate an ‘asthmatic constitution’. Similarly, occupational and environmental irritants may be risk factors, but especially so in individuals who smoke. Target populations for whom spirometry screening is recommended are listed in Table 2.
Table 2. Target populations for spirometry screening
Category: Chronic obstructive
Tags: Chronic obstructive pulmonary disease, Screening, Spirometry
© 2011 - 2024 buy-asthma-inhalers-online.com. All rights reserved.